Click the link to purchase on Amazon 🎉📚
==============================================
🎥 Check Out All Videos at Once! 📺
👉 Visit Visualizing MSK Blog to explore a wide range of videos! 🩻
https://visualizingmsk.blogspot.com/?view=magazine
📚 You can also find them on MSK MRI Blog and Naver Blog! 📖
https://www.instagram.com/msk_mri/
Click now to stay updated with the latest content! 🔍✨
==============================================
📌Osgood-Schlatter Disease Overview
✅ Introduction
- Osgood-Schlatter disease is a common condition in active male adolescents, caused by repetitive stress on the patellar tendon at its insertion on the tibial tuberosity.
- It often affects those involved in jumping, squatting, and kicking activities and can be bilateral in up to 50% of cases.
- Common in Active Adolescents: Particularly those involved in high-impact sports.
- Bilateral Occurrence: Up to 50% of cases can affect both knees.
- Spontaneous Healing: Most patients heal over time, although symptoms can persist.
✅ Pathophysiology
- The tibial tuberosity's weak apophyseal cartilage can't withstand the strong forces from the quadriceps muscles.
- Initially, the tubercle develops from fibrocartilage, providing strength.
- As it matures and ossifies, it converts to weaker columnar cartilage, increasing injury risk.
✅ Imaging Findings
- Fragmentation and edema of the tibial tubercle.
- Thickening and increased signal of the patellar tendon distally at the level of the tibial tubercle.
- Irregularity of the tibial tubercle, often persisting into adulthood.
- Calcification and thickening of the patellar tendon.
- Irregular ossification of the tibial tubercle and overlying soft-tissue swelling.
- Reactive secondary heterotopic bone formation at the patellar tendon insertion site, resulting in a visible and painful bump.
✅ MRI Findings
- Fragmentation and edema of the tibial tubercle with surrounding soft tissue edema.
- Thickening of the patellar tendon with increased signal distally at the level of the tibial tubercle.
- Transverse clefts in the damaged ossifying cartilage.
- Bone fragmentation and disordered ossification during the healing stage.
- Displaced ossicles, enlargement, and altered signal intensity of the patellar tendon, marrow, and soft-tissue edema at the tuberosity in chronic active cases.
✅ Stages of Osgood-Schlatter Disease
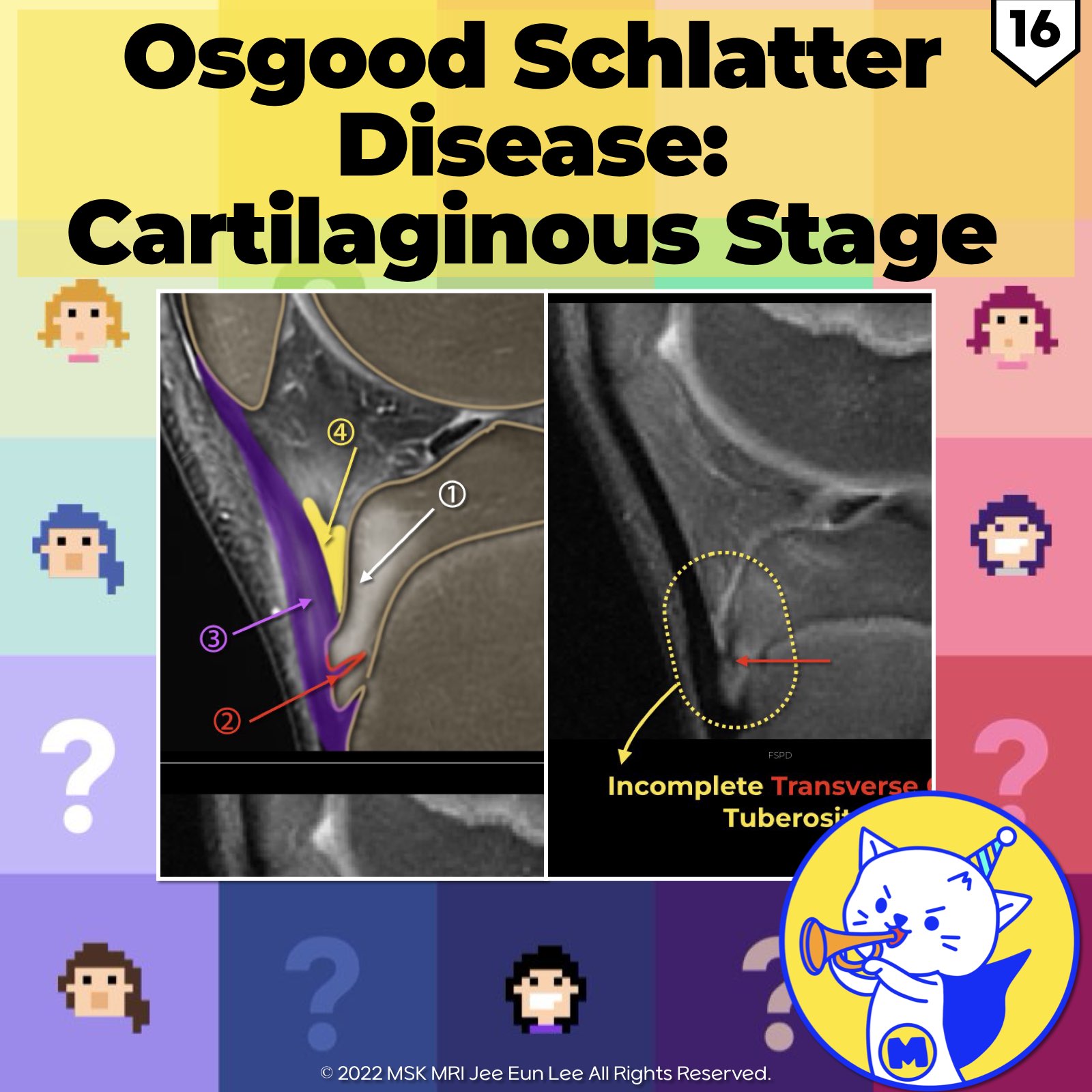
1️⃣ Cartilaginous Stage:
- Soft-tissue findings dominate, including tendon thickening, prepatellar edema, and deep infrapatellar bursitis.
- Transverse clefts in the secondary ossification center of tuberosity
2️⃣ Healing Stage:
- Bone fragmentation and disordered ossification become apparent on radiographs.
- Most patients undergo spontaneous healing, and the bone fragments reunite with the tibia, even if symptoms persist.
3️⃣ Chronic Active Stage:
- Displaced ossicles, altered signal intensity of the patellar tendon, marrow and soft-tissue edema, and a chronically distended deep infrapatellar bursa are observed.
- Unstable avulsed fragments can displace proximally, forming symptomatic nonunited ossicles and often leading to chronic symptoms into adulthood.
References
RadioGraphics 2018; 38:2069–2101
RadioGraphics 2009; 29:877–886
Magn Reson Imaging Clin N Am 22 (2014) 601–620
"Visualizing MSK Radiology: A Practical Guide to Radiology Mastery"
© 2022 MSK MRI Jee Eun Lee All Rights Reserved.
No unauthorized reproduction, redistribution, or use for AI training.
#OsgoodSchlatterDisease, #KneeInjury, #OsgoodSchlatterDisease, #KneePain, #YouthSports, #AdolescentInjuries, #TibialTuberosity, #PatellarTendonitis, #OrthopedicHealth, #SportsInjuries, #Radiology, #PhysicalTherapy
'✅ Knee MRI Mastery > Chap 4BCD. Anterior knee' 카테고리의 다른 글
| (Fig 4-B.18) Osgood Schlatter Disease: Chronic Active Stage (1) | 2024.06.15 |
|---|---|
| (Fig 4-B.17) Subchondral Fracture vs. Osgood Schlatter Disease (0) | 2024.06.15 |
| (Fig 4-B.15) Patellar Tendon Partial Tear (0) | 2024.06.12 |
| (Fig 4-B.14) Patellar Tendinosis (0) | 2024.06.12 |
| (Fig 4-B.13) Traumatic Separation of Prepatellar Quadriceps Continuation (0) | 2024.06.12 |